What Does Avs Failure Mean?
What is AVS Failure?
AVS stands for aortic valve stenosis, which is a narrowing of the aortic valve opening that restricts blood flow from the left ventricle to the aorta (https://openmd.com/define/aortic+valve+stenosis). The aortic valve is one of four valves in the heart that keeps blood flowing in the proper direction. It opens to allow oxygen-rich blood to flow from the left ventricle into the aorta, and then closes to prevent blood from flowing backward into the left ventricle.
In AVS failure, the aortic valve opening becomes increasingly narrowed or stiffened, which obstructs the flow of blood from the heart into the aorta. As the aortic valve narrowing progresses, the left ventricle has to work harder to pump blood out through the restricted valve opening. This results in pressure and volume overload on the left ventricle and left atrium (https://www.ncbi.nlm.nih.gov/medgen/C0003507). If left untreated, AVS can lead to left ventricular hypertrophy, heart failure, syncope, and angina.
AVS failure is caused by age-related degenerative calcification and progressive fibrosis of the valve leaflets. Risk factors include advanced age, congenital bicuspid aortic valve, and conditions associated with accelerated calcification. The main symptom is exertional dyspnea, along with syncope and anginal chest pain in severe cases. Diagnosis involves imaging tests like echocardiography to evaluate valve structure and function.
Causes of AVS Failure
Aortic valve stenosis is typically caused by age and general wear and tear on the valve over time. As people get older, the valve can become stiff or fused from calcium deposits that build up on the valve flaps, preventing them from opening fully. This progressive calcification is by far the most common cause of aortic stenosis in adults over 50 years old. It occurs slowly over many years. (1)
Some people are born with a defective or abnormal aortic valve that does not function properly. This congenital defect accounts for a small percentage of aortic stenosis cases and may require valve repair or replacement surgery at a young age. (2)
A small number of aortic stenosis cases are caused by damage to the valve from rheumatic fever, an inflammatory disease that can develop after a strep throat infection. Rheumatic fever can cause scarring and fusion of the valve flaps. This cause is less common in developed countries today due to prevention and treatment of strep throat. (3)
Symptoms
Aortic valve stenosis (AVS) can cause a variety of symptoms. Some of the most common include:[https://www.mayoclinic.org/diseases-conditions/aortic-stenosis/symptoms-causes/syc-20353139]
Chest pain – AVS can cause chest pain or tightness due to reduced blood flow to the heart muscle.[https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-aortic-valve-stenosis]
Shortness of breath – The heart has to work harder to pump blood through the narrowed valve, which can lead to shortness of breath, especially with exertion.
Fatigue – The extra effort needed for the heart to pump blood can cause unusual tiredness and fatigue.
Heart murmur – The turbulent blood flow through the narrowed aortic valve causes a heart murmur that your doctor can hear with a stethoscope.
Fainting – Some individuals with severe AVS may faint or feel lightheaded as their heart struggles to pump sufficient oxygenated blood to the brain.
Diagnosis
To diagnose aortic valve stenosis, doctors will perform a physical exam in addition to several tests like an echocardiogram or cardiac catheterization. The physical exam provides important initial clues to help determine if stenosis is present [1].
An echocardiogram, also called an echo, is typically the next test ordered if stenosis is suspected during a physical [2]. This non-invasive test uses ultrasound waves to produce images of the heart’s valves and chambers, allowing doctors to see abnormalities in the aortic valve. The echo can evaluate the severity of stenosis and its impact on heart function.
If further confirmation is needed, a cardiac catheterization can definitively diagnose stenosis and measure the pressure gradient across the aortic valve [1]. This more invasive test threads a thin tube into the heart’s chambers and valves. Dye is injected to visualize the heart’s structures via X-ray as measurements are taken.
Together, the physical exam, echocardiogram, and potential cardiac catheterization provide the information needed to confirm an aortic valve stenosis diagnosis.
Treatment
Treatment for AVS depends on the severity of stenosis and symptoms. Mild stenosis often doesn’t require treatment. Moderate to severe stenosis usually requires treatment to prevent complications.
Medications can help relieve symptoms but don’t treat the underlying cause. Drugs that relax and open blood vessels, such as nitroglycerin, can temporarily ease symptoms. High blood pressure medications like ACE inhibitors or diuretics may also help.
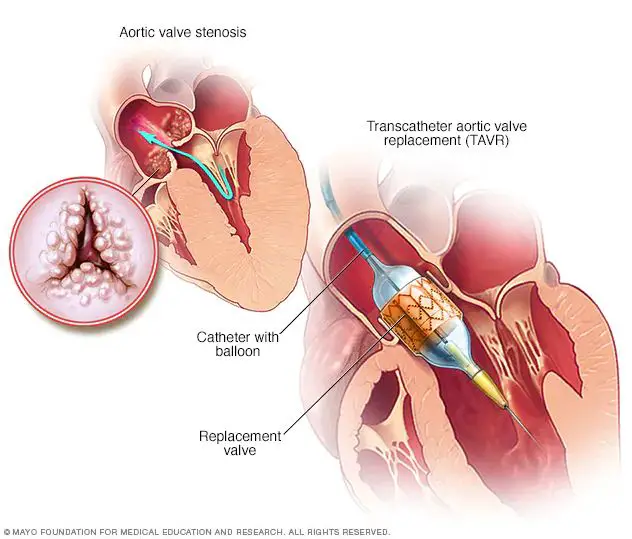
When stenosis is severe, the aortic valve needs to be repaired or replaced. Valve replacement surgery is the main treatment. The diseased valve is removed and replaced with an artificial heart valve. Two types of valve replacement procedures are:
- AVR (aortic valve replacement) – open heart surgery to remove the valve and implant an artificial one
- TAVR (transcatheter aortic valve replacement) – a minimally invasive procedure where a catheter is used to insert a new valve without open heart surgery
Balloon valvuloplasty is another less invasive treatment option. A surgeon threads a catheter with a small balloon at the tip through a blood vessel to the valve. The balloon is inflated to stretch open the valve. This can provide temporary relief and delay the need for surgery in some patients.
Cited from: https://www.mayoclinic.org/diseases-conditions/aortic-stenosis/diagnosis-treatment/drc-20353145
Lifestyle Changes
Making certain lifestyle changes can help manage symptoms and slow the progression of aortic valve stenosis. The most important behavior modifications to make include:
Diet and Nutrition
Following a heart-healthy diet is recommended for aortic valve stenosis. This includes:
- Eating plenty of fruits, vegetables, and whole grains
- Choosing lean protein sources like fish, poultry, beans, and nuts
- Avoiding processed foods high in trans fats, saturated fats, salt, and sugar
- Staying well-hydrated by drinking adequate water
Some research indicates that certain dietary supplements like magnesium, coenzyme Q10, and omega-3 fatty acids may be beneficial. However, more studies are needed to confirm these effects.
Exercise
With doctor approval, light to moderate intensity exercise can be incorporated provided symptoms are stable. This may involve walking, swimming, stationary biking, or other low-impact activities. However, overexertion should be avoided.
Managing Other Conditions
Controlling any coexisting conditions like high blood pressure, high cholesterol, or diabetes is essential. Following all treatment plans for these diseases can ease the burden on the heart.
Prognosis
The prognosis for aortic valve stenosis depends significantly on the severity of the condition. According to the Mayo Clinic, severe aortic stenosis is life-threatening, with about 50% of patients dying within 2 years if left untreated. Moderate aortic stenosis has a better prognosis but can still worsen over time. Mild aortic stenosis may not progress or cause issues for many years.
Early diagnosis and treatment is critical for improving prognosis. The Cleveland Clinic notes that prompt aortic valve replacement surgery in patients with severe aortic stenosis can restore normal lifespan. Medications can help mild-moderate cases. Lifestyle changes like diet and exercise may also slow progression. Overall, the earlier aortic valve stenosis is caught, the better the outcomes.
Prevention
While aortic stenosis often can’t be prevented, you can take steps to reduce your risk of developing it. Here are some tips for prevention:
Manage risk factors. Controlling high blood pressure, high cholesterol and diabetes can help reduce your chances of developing aortic stenosis. Eat a heart-healthy diet, exercise regularly, maintain a healthy weight and take medications as prescribed by your doctor.
Get routine checkups. See your doctor for regular physical exams and report any symptoms such as chest pain, dizziness or shortness of breath. Detecting a heart valve problem early provides the best opportunity for effective treatment.
Your doctor may recommend imaging tests such as an echocardiogram to check for aortic valve thickening or stenosis, even if you have no symptoms. Finding and treating valve problems early is important to prevent complications.
Outlook and Future
While surgical aortic valve replacement (SAVR) has been the standard treatment for severe aortic stenosis for many years, less invasive transcatheter aortic valve replacement (TAVR) is becoming more common, especially for high-risk patients. According to a study in the New England Journal of Medicine, TAVR results in lower rates of death and disabling stroke compared to SAVR.
Ongoing research is looking at improving TAVR techniques and expanding its use to lower-risk patients. There is also research into new valve designs and materials to improve durability and reduce complications. Other areas of research include identifying genetic and environmental factors related to calcific aortic valve disease to help prevent it from developing in the first place.
With continued advances in less invasive techniques and valve technology, the outlook for treating aortic stenosis is expected to keep improving in the years ahead.
Conclusion
In summary, aortic valve stenosis is a condition where the aortic valve narrows and prevents blood from flowing normally from the left ventricle into the aorta. The causes include age-related degenerative calcification, rheumatic fever, or congenital abnormalities. Symptoms like chest pain, dizziness, and shortness of breath tend to appear once the stenosis becomes severe. AVS is diagnosed through physical exams, electrocardiogram, echocardiogram, and cardiac catheterization. Treatment depends on the severity and typically involves either valve repair, valve replacement through open heart surgery, or transcatheter aortic valve replacement. Lifestyle changes like maintaining a healthy weight and controlling other heart conditions are also recommended. While stenosis tends to progress over time, following doctor’s orders and adhering to lifestyle changes can help slow the progression. Early diagnosis and proper management of AVS are crucial for improving prognosis and preventing complications like heart failure, cardiac arrest, or death.